BASICS
The Building Adaptive School-based Interventions for Caries (BASICS)
Dental caries is the world’s most prevalent noncommunicable disease, and is highly inequitable. To combat this silent epidemic, school-based caries prevention can increase access to critical care for underserved populations, reducing caries risk and mitigating its severe health and socioemotional consequences. However, despite the use of evidence-based interventions, approximately 30% of children participating in school-based caries prevention fail to respond to treatment, developing new caries and remaining at high risk for subsequent complications.
Our etiologic investigations into the determinants of treatment nonresponse demonstrated that there are innate microbial and environmental factors that may be related to nonresponse to school-based care, identifying significant differences between responders and nonresponders at phylum and genus levels.
From this research, we combined data from the oral microbiome, clinical observations, and hygiene behaviors and developed an artificial neural network that can be used to predict treatment nonresponse.
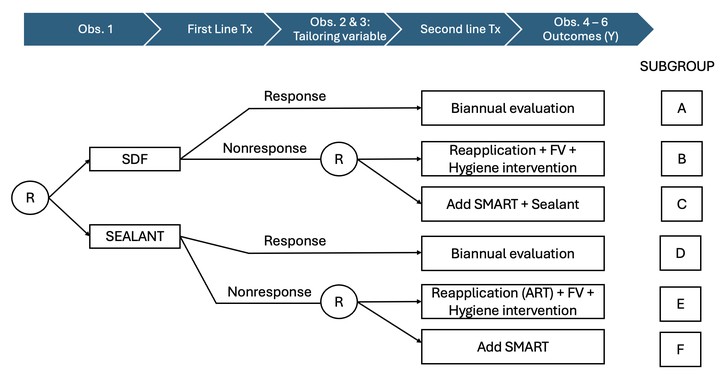
Additionally, the sustainability of school-based prevention is jeopardized due to prohibitive costs, limitations of the professional workforce, and relying on treatments that are not optimized for individual patient needs. We propose to develop and assess personalized, resource-efficient approaches to school caries prevention using adaptive interventions, leading to improvements in both oral health and oral health equity. Evaluated by embedding dynamic treatment regimes (DTR) within a sequential multiple assignment randomized trial (SMART) design, we will explore a number of hypotheses related to adaptive preventive interventions. First, we will test the effects of adaptive interventions on reducing treatment nonresponse using generalized linear mixed models, followed by identifying the best dynamic treatment regime using augmented inverse probability weighted marginal structural models for causal effect estimation. We will subsequently build an optimal adaptive intervention using Q-learning, tailoring treatments to individual patient attributes and responsiveness. We will conclude with a microcosting analysis of the adaptive interventions, ultimately quantifying the intervention costs under different implementation scenarios and taking the first step towards understanding how much payers should reimburse for adaptive interventions. To facilitate completion of these aims, we will implement our adaptive prevention model in the PRISMS network: a multistate community-based participatory research group of schools serving predominantly high-risk children that are committed to innovative approaches to caries prevention. This will simplify site and patient recruitment, embeds community engagement into our research process, and has a demonstrated history of both successful clinical care and research. Successful completion of this project will produce a resource-efficient adaptive prevention intervention (API) to reduce treatment nonresponse, improving both oral health and oral health equity.
BASICS is funded by the NIMHD.